A New Benchmark
The healthcare landscape is continuously evolving, and innovative collaborations are often at the heart of transformative changes. One such collaboration that has garnered attention for its success is the partnership between CPESN® Iowa pharmacies and Elevance Health/CarelonRx. This partnership, aimed at improving the care and lowering the cost of high-risk Medicaid members, has set a new benchmark in integrated care delivery, demonstrating the profound impact that community pharmacies, health plans, and pharmacy benefit managers (PBMs) can have when they work together effectively.
A Game-Changing Pilot Program
Over the course of a two-year pilot program, CPESN Iowa pharmacies engaged with high-risk Medicaid members, leading to a significant 33% reduction in inpatient admissions. This remarkable decrease highlights the efficacy of proactive pharmacy involvement in managing patient care and preventing costly hospitalizations. Lindsey Ludwig, Executive Director of CPESN Iowa, captures the essence of this success in a short video from the Payer, Purchaser, Partner Success series, which details the real-world benefits and positive changes brought about by CPESN pharmacies.
The pilot program’s success is a testament to how well-coordinated efforts between CPESN pharmacies and health plans, and other payers can yield tangible improvements in patient outcomes and cost management. Integrating community pharmacies into Medicaid strategies has enhanced patient care and shown the potential for substantial cost savings.
Insights from Research
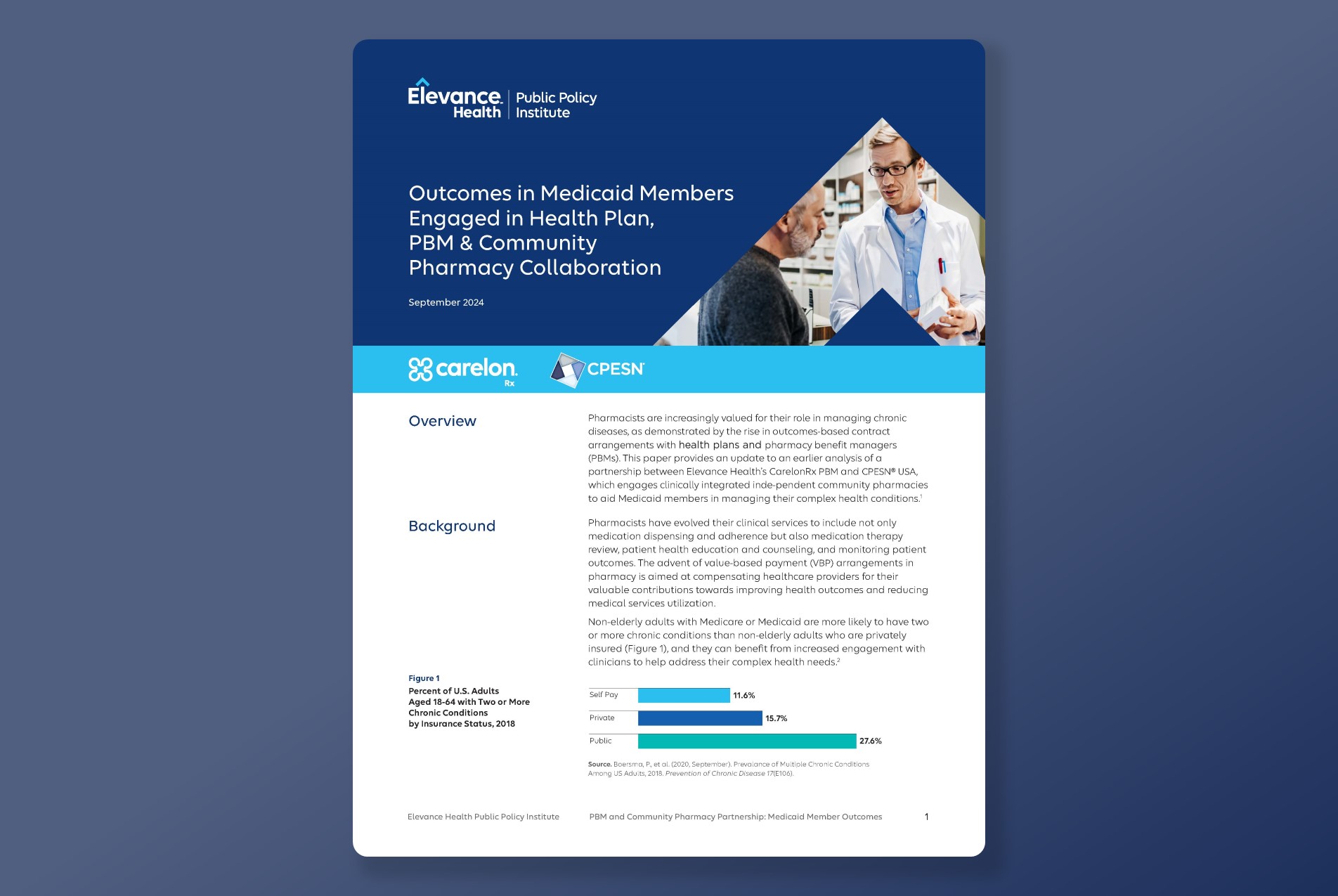
The Elevance Health Public Policy Institute’s recent paper, “Outcomes in Medicaid Members Engaged in Health Plan, PBM & Community Pharmacy Collaboration,” provides a retrospective analysis of the claims data. Key findings from the research include:
- Reduction in Medical Service Utilization: CPESN-engaged members in Iowa experienced a 33% reduction in medical service utilization related to their chronic conditions, in stark contrast to the increased utilization observed in nonparticipant members.
- Enhanced Care Quality: Members engaged with CPESN pharmacies showed a higher rate of HEDIS (Healthcare Effectiveness Data and Information Set) gap closures compared to their nonparticipant counterparts, indicating improved quality of care.
- Cost Savings: The program led to significant reductions in medical costs associated with chronic conditions, reflecting the cost-effectiveness of this value-based care model.
This is the second paper from the Elevance Health Public Policy Institute to highlight the value of CPESN pharmacies. The first, “PBM and Community Pharmacy Partnerships Can Improve Medicaid Outcomes” published in October of 2023, reported a 30% reduction in hospitalization costs and an 18% reduction in emergency department related costs for patients in the CPESN and CarelonRx program.
Looking Forward
Pharmacist and pharmacy owner Alison Haas, CPESN USA Director of Value-Based Contracting, emphasizes the scalability of this program, citing Iowa as a prime example of its potential. “This program continues to scale because of the great work of pharmacies and local networks participating in the program.” Haas notes. Currently, Elevance Health/CarelonRx is actively working with 11 different CPESN networks across the U.S., with plans to extend the partnership further in the coming year.
To ensure continued shared success, a quarterly all-pharmacy call brings together leaders from both CPESN Networks and Elevance/CarelonRx to discuss wins, opportunities, and best practices for enhancing patient care.
By recognizing and rewarding CPESN pharmacies for their role in managing chronic conditions and achieving cost savings, this value-based arrangement fosters a more effective and efficient healthcare system. The success of CPESN Iowa, as documented by the Elevance Health Public Policy Institute, demonstrates the potential for these innovative collaborations to transform care delivery and improve outcomes for high-risk patients managing chronic conditions.